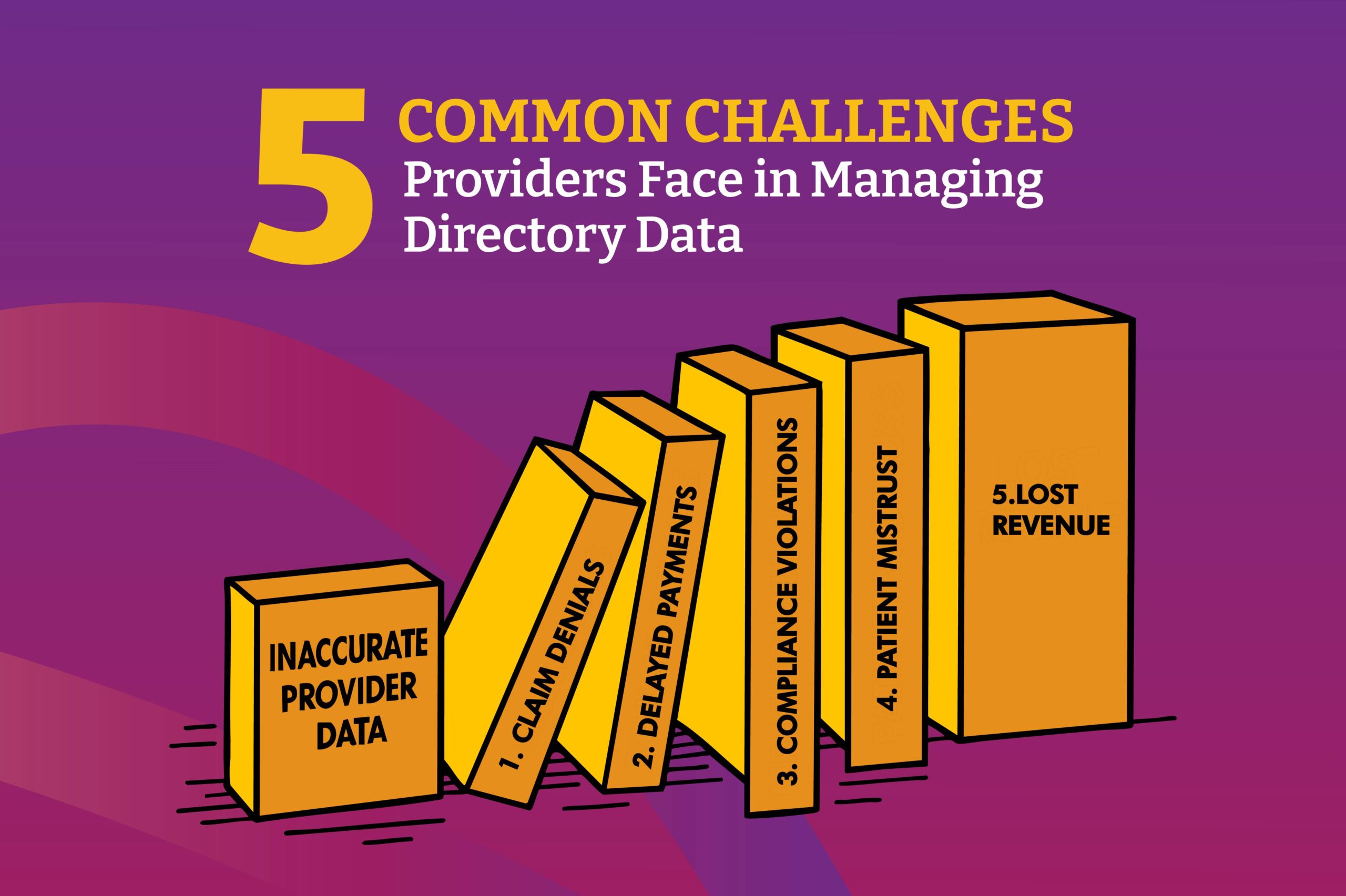
5 Common Challenges Providers Face in Managing Directory Data
Accurate provider directory data is foundational to a functioning healthcare system. It fuels everything from scheduling and referrals to claims and care coordination. But for payers and providers alike, managing that data has become a high-stakes challenge. Incomplete, outdated, or inconsistent directory data affects compliance, delays payments, and erodes patient trust.
Below, we break down the most pressing issues in provider directory data management—and what healthcare organizations can do to solve them.
What Is Provider Directory Data Management?
Provider directory data management refers to the process of maintaining and updating key information about healthcare professionals. This includes names, credentials, NPI numbers, accepted insurance plans, locations, specialties, and licensure.
It’s essential for both payers and patients. For payers, accurate provider data supports eligibility verification, claims processing, and compliance with CMS and state requirements. For patients, it ensures they can find the right doctor in the right network at the right time.
Why Managing Provider Data Is Increasingly Complex
Healthcare data isn’t just growing—it’s splintering. A single provider might be affiliated with multiple facilities, payer networks, and billing systems. Add to that a growing list of stakeholders, evolving state and federal regulations, and the lack of universal data standards, and it’s no wonder the problem is escalating.
Payers and providers are often stuck reconciling inconsistent inputs across EHRs, credentialing systems, third-party vendors, and internal spreadsheets—each with different formats and update cycles.
The 5 Most Common Challenges in Provider Data Management
1. Inconsistent Data Across Systems
Internal systems and external partners often record provider data in different formats or levels of detail. One directory may list a physician under their full name and board certifications, while another lists only a partial address and practice name. These discrepancies create mismatches, duplicate records, and incorrect listings, ultimately leading to misinformation reaching patients.
2. Manual and Time-Consuming Workflows
Many organizations still rely on spreadsheets, emails, and outdated tools to manage provider data. These manual workflows are error-prone and time-intensive, often delaying updates or creating bottlenecks. When staff are stuck chasing down data corrections, it diverts time from higher-value tasks and contributes to administrative fatigue.
3. Ensuring Data Accuracy and Completeness
Key fields are often left blank, including specialties, languages spoken, or participation in certain insurance plans. In other cases, outdated certifications or licenses linger in the system long after expiration. Without automated validation and alerts, it becomes nearly impossible to maintain accuracy at scale.
4. Frequent Provider Changes
Providers regularly change networks, retire, relocate, or switch specialties. Without a centralized, proactive update process, these changes can take weeks or even months to reflect across systems. In the meantime, claims can be denied, referrals misdirected, and directories rendered unreliable.
5. Lack of Interoperability Across Systems
Too often, EHRs, CRMs, credentialing databases, and payer portals don’t speak the same language. This lack of interoperability prevents organizations from sharing updates in real time or creating a single, authoritative view of provider records. The result: siloed data, versioning conflicts, and a fragmented experience for providers and patients alike.
The Cost of Poor Provider Data Management
Errors in provider directory data have ripple effects. Non-compliance with CMS directory accuracy standards can lead to steep fines. Incorrect or outdated data leads to claim denials, delayed payments, and loss of revenue. Perhaps most damaging, it degrades trust with both patients and providers, who expect accurate information and frictionless experiences.
Best Practices for Improving Provider Directory Data Management
- Centralize your data into a single source of truth across teams and systems.
- Automate data validation using APIs, alerts, and AI-driven tools.
- Enable real-time updates through bidirectional integrations with core platforms like EHRs, CRMs, and payer portals.
- Establish governance across compliance, IT, and clinical teams to align data ownership and accountability.
- Perform regular audits and implement hygiene protocols to flag outdated or duplicate entries before they become systemic issues.
At Madaket, we help payers and provider organizations automate these critical workflows. Explore our Provider Directory Data Management service to learn more.
The Bottom Line
Provider directory data management isn’t just a back-office task—it’s a strategic priority. As provider networks grow and regulations tighten, healthcare organizations must invest in systems that make data accuracy sustainable.
The future of care coordination, reimbursement, and patient satisfaction hinges on trustworthy data. Now is the time to prioritize it.
© 2024 Madaket Health | Privacy Policy | Terms & Conditions
