A Platform That Works the Way Provider Data Should
Healthcare loses $250 billion annually to administrative waste, and bad provider data is a key driver. Inaccurate directories, outdated rosters, and siloed systems lead to claim denials, revenue loss, compliance risks, and suboptimal patient and member experiences.
Madaket was built to solve this.
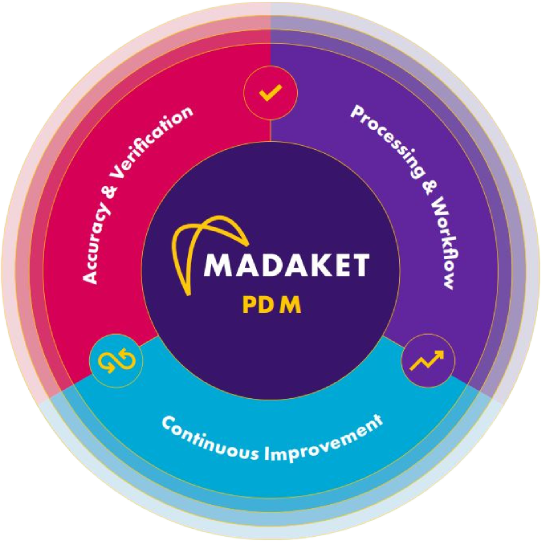
Our SOC 2 Type 2-compliant platform continuously ingests, standardizes, validates, and synchronizes provider data, transforming a chronic liability into a strategic and reliable asset.
We don’t just clean data once. We maintain an always-on feedback loop that ensures data is complete, accurate, and up-to-date, reducing manual work, improving outcomes, and supporting compliance.
Sitting at the heart of the provider–payer ecosystem, Madaket captures the most important provider data, links it to transactions, affiliations, and payments, and delivers it as a trusted source of truth.
This is not just provider data management.
This is provider data, solved.
Why Madaket?
More than 80% of U.S. provider groups rely on Madaket for essential operations. Our platform enhances data integrity and submission speed, without increasing headcount.
Provider Data Exchange (PDX)



EDI/EFT Enrollments
A platform for (all) the people.
We partner with all, compete with none.